|
The 4 Types of PCOS - authored by Dr Sarah DiMunno ND
If you are reading this article, you probably already know or suspect that you have PCOS, which stands for Polycystic Ovarian Syndrome. If you are thinking, “What the heck is that?” here is some background information. PCOS is a very common women’s health condition that leads to hormonal imbalances and a loss of ovulation. It is the number one reason women are diagnosed with infertility; and because of this it makes up a large portion of my practice. Diagnosis requires 2 of the following criteria:
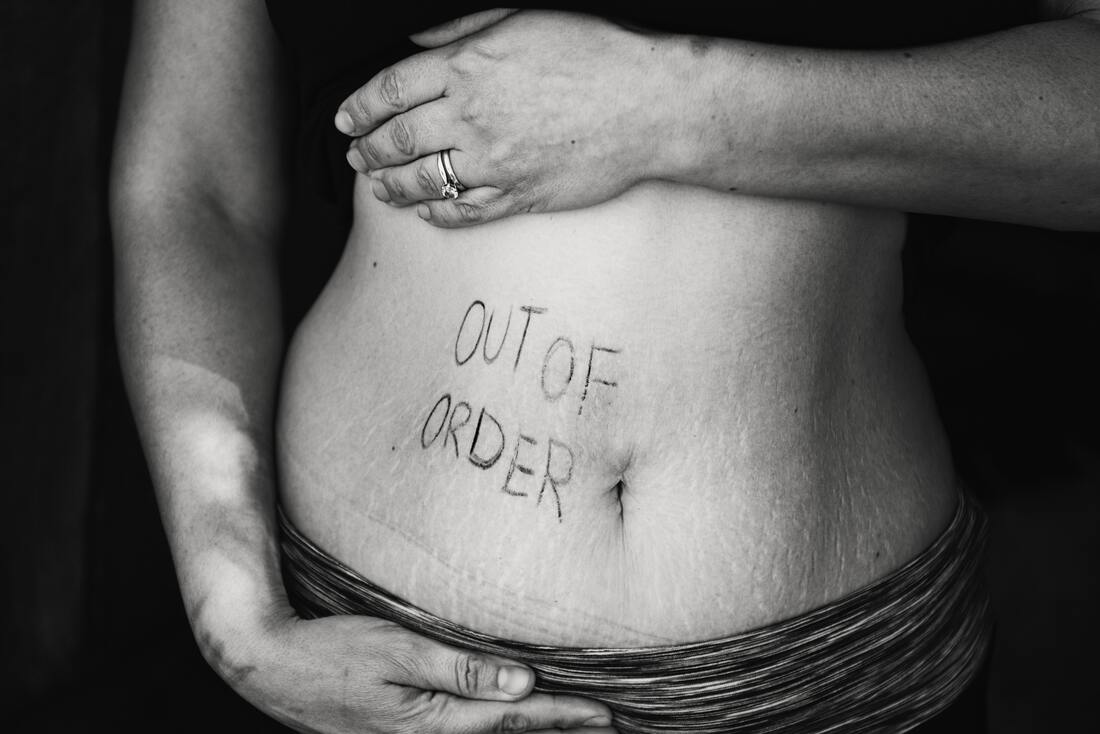
Although not a diagnostic criteria the inability to lose weight deserves an honourable mention, and you’ll find out why a little later. As you can see the name of the condition is slightly misleading, you don’t necessarily need cystic ovaries to be diagnosed. Because of this misnomer many people focus too much on the presence or lack of cysts on the ovaries. Having cysts on their own isn’t enough to diagnose PCOS and you can still have PCOS if you don’t have cysts on your ovaries. If you were experiencing signs of high testosterone, also known as androgen excess, and a lack of ovulation, I’d be thinking about diagnosing PCOS regardless of cysts. If you do fit the criteria, the good news is this condition is 100% treatable. Figuring out the type of PCOS you have is the key to successful treatment. There are four types of PCOS, each with a slightly different root cause, making treatment approaches variable as well. Lucky for you, I’ve broke down each type below: Insulin-Resistant PCOS This is by far the most common and classic driver behind PCOS. Insulin is the hormone that is released in our body after eating; it brings blood sugar levels down. However, when you have insulin resistance your body doesn’t respond to the insulin released, and as a result your body starts producing more and more to keep your blood sugar levels normal. If you are susceptible to PCOS, these high levels of insulin will start preventing ovulation, make ovaries produce testosterone over estrogen, and boost luteinizing hormone (LH), which further reinforces the imbalance. If you have insulin-resistant PCOS, you have all the criteria of PCOS plus insulin resistance. You know you have insulin resistance if you struggle with maintaining a healthy weight and/or by measuring both your fasting blood sugar and fasting insulin in blood work. It’s important to address your insulin resistance because too much insulin can impair not only your cycle but can also contribute to heart disease, osteoporosis, and diabetes. Addressing insulin resistance is similar to treating diabetes and will respond very well to lifestyle changes like diet and exercise. Post-Pill PCOS This occurs after you stop taking birth control. To determine whether this is the type of PCOS you have, it is very important to take a look at what your period looked like prior to and following the birth control pill. If your period was irregular prior to starting the pill, you likely had PCOS the entire time, and didn’t know because the pill was masking your symptoms. If your period was normal, then your symptoms might be due to the pill and should return back to normal function after some time. It’s still important to investigate insulin resistance here because the pill can cause or worsen insulin resistance. If insulin resistance is present, then you have insulin resistant PCOS and should follow the instructions above. If insulin resistance is absent, then you can assume that with time and patience your hormones will return to normal. However, there are some things you can do to help ease the transition, including consuming adequate calories, and perhaps support a regular cycle using herbs or acupuncture. Inflammatory PCOS If you don’t have insulin resistance or the pill hasn’t negatively affected your periods, and you still have symptoms of PCOS then you might have inflammatory PCOS. This type of PCOS occurs when there is a lot of inflammation present in the body and past exposure to environmental toxins (who hasn’t been, am I right?!). Signs and symptoms of inflammation in the body include: IBS, unexplained fatigue, headaches, joint pain, and skin conditions like eczema and psoriasis. As you might have guessed the main goal for treating this type of PCOS is decreasing overall inflammation. Adrenal PCOS Lastly, if you don’t fit the criteria from any of the above categories then you might have adrenal PCOS. Chances are if you have this type of PCOS you are under A LOT of stress and you have been for some time (any professional students out there?). During the stress response, cortisol, our stress hormone, is released from the adrenal glands. DHEAS, another adrenal hormone, rises as cortisol does leading to high levels of DHEAS. When DHEAS is elevated, it can cause androgen excess as seen in PCOS. You should consider Adrenal PCOS if DHEAS is the only evidence of elevated androgen found and all other male sex hormones are normal. If you have this type of PCOS, you likely have a whole other whack of symptoms related to chronic stress like waking at night between 2-4 am, non-stop bloating, brittle nails and hair, low energy, etc. Since, this type of PCOS is largely driven by an abnormal stress response, treatment focus is on major stress reduction. If you feel like you don’t quite fit any of the descriptions above but have irregularities in your menstrual cycle, don’t fret. There are a number of other things to investigate including vitamin deficiencies & other hormonal imbalances that weren’t mentioned in this article. I offer a free consultation to all new patients. Book today to come in and see me for a free 30 minute consultation. We can discuss any questions you might have and I can give you some options for treatment.
4 Comments
|
Copyright © Toronto Reproductive Acupuncture Clinic. All Rights Reserved | Privacy Policy


 RSS Feed
RSS Feed