|
Authored by: Jennifer Dickey, Registered Acupuncturist Oh, the holiday season. That time of year for get-togethers, gift purchases, food, and cheer. Tis the season to be merry, but for a lot of people, it's the time for stress levels to skyrocket! As great as it is, the holidays can also be a difficult time, particularly for individuals and couples dealing with infertility.
The constant social & family gatherings and children’s excitement centered around this time of year can intensify the emotional ups and downs that come with fertility struggles. Here are a few suggestions to help you navigate through the holidays and remember, it’s okay to prioritize your emotional well-being and take the necessary steps to cope with these challenging times. JUST SAY NO It’s often hard to say no when those party invites come out, but give yourself the gift of boundaries this holiday season! You are not obligated to anybody but yourself and your mental and emotional well-being. Ask yourself if an event might trigger negative emotions and consider how it may or may not impact you. Don’t be afraid to decline invitations and stick to the events you know you’ll have fun at. Start a new holiday tradition. Maybe stay in and be cozy watching movies with your partner, or if you’re feeling social, spend time with people who will make you feel good about where you’re at. BE PREPARED If you feel that there is no way you can skip out on an event give yourself some time to prepare ways to feel you have control over your circumstance. Bring a support person to help if you feel overwhelmed, or to help if you need to make a quick exit. Have some canned responses ready If you have a prying family member who may be there. CONNECT WITH YOUR SUPPORT SYSTEM If you’re feeling particularly vulnerable this time of year, seek support from loved ones you’ve confided in to help deflect any awkwardness or unsolicited comments when you attend a gathering. If you’ve kept your journey private, you can always reach out to a fertility support group or perhaps a therapist or other practitioner you’ve been seeing. You don’t have to deal with this alone. TAKE A BREAK Take a short break from it all (unless you’re already on a schedule). Sometimes it's nice to just feel like “yourself” again and not hyperfocus on timing, what you’re eating, and all the medication. Have that second helping of dessert and a glass of cheer. Allow yourself to feel more at ease during this time of year. MAKE TIME FOR SELF-CARE Be kind to yourself. Limit your obligations, and be selective of what events you commit to. Carve out more time to do the things that bring you joy, whether that’s working out, eating some good food, or taking a bath with a book. Treat yourself to a day at a spa, or hangout with a friend. Book a massage or Acupuncture session to help with stress. Give yourself a gift this year - you deserve it!
0 Comments
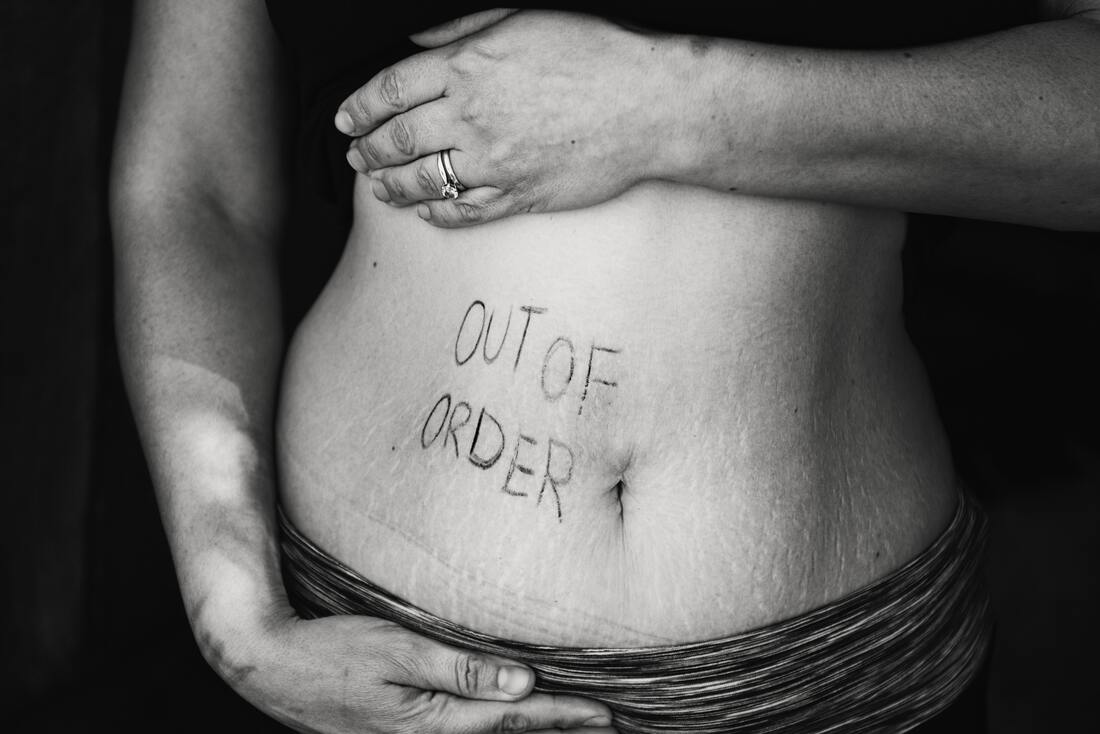
Authored by; Chelsea Wall, Registered Massage Therapist Taking the time to treat yourself and give your body and mind a break (even momentarily) can help the way you see and appreciate your body, especially while navigating the trials and tribulations of trying to conceive, or experiencing the aches and pains of pregnancy. Massage therapy can help no matter where you are on your journey to parenthood! Here are some of your most common fertility/pregnancy massage questions answered!
1. How can a massage benefit my fertility? Massage can increase blood circulation to the ovaries and uterus, support lymphatic drainage, which aids in eliminating waste and toxins from your body, benefit sleep quality, and most importantly reduces stress by decreasing cortisol levels and increasing serotonin and dopamine which helps support our body’s hormone functions and our ability to ovulate and maintain a healthy pregnancy. 2. Can I still get a massage if I’m doing IVF? Absolutely you can!!! The IVF process can take a heavy emotional and physical toll on you, and what better way to mitigate that tension than a massage that can benefit your mind and your body? On top of reducing your stress and anxiety, massage therapy can help support pelvic blood to help with follicular growth and support your uterine lining! It can also provide relief from some of the nasty side effects the fertility medication such as bloating, headaches, nausea, insomnia, mood swings, and back pain. Massage therapy is safe at any time of your IVF journey although It is highly recommended to avoid any deep abdominal pressure during your stimulation phase due to the enlargement of the ovaries and to avoid pressure on certain areas of the body during your 2-week wait. 3. When’s the best time for a fertility massage? If you’re trying to conceive naturally, the best time for a fertility-focused massage to maximize pelvic blood flow would be anytime after your bleeding phase and before ovulation. If you and your partner have had intercourse during your ovulation massage techniques on the abdomen would be avoided, and focus would be more geared towards stress and tension, and other areas of the body that can aid in supporting uterine health such as the lower back, hips, and legs. If you’re preparing to start your family in the near future, or you’re waiting for that fertility clinic to call you back it’s a good idea to start optimizing your body by getting regular massages 90 days prior to best optimize your body for conception, along with other healthy lifestyle changes, good quality supplements, and regular Acupuncture! 4. Do I have to be trying to conceive to get a massage from you? Absolutely NOT! sometimes it's nice to just remove yourself and take a break from all the fertility stuff and just get a nice relaxing massage to ease stress or to work out any muscle tension you may be having! 5. What can I expect from a massage? When you come to get a massage, your appointment is completely your own. As each individual is different, where you are feeling your pain, your stress, or your tension will be different than someone else who may be in a similar position to you. You are in charge of your appointment. We will discuss beforehand to see how you are feeling and figure out how I can help you feel your best. I will ask for your feedback during your appointment and check-in to ensure you are enjoying your appointment and you are comfortable the entire time you are on the table. 6. Once I’m pregnant, is a massage safe? Once you are pregnant, there are certain positions that we will avoid. We will not have you lie on your stomach after the first trimester and will avoid lying flat on your back as well from that point on. I will ensure your body is supported by pillows and you are comfortable with your positioning. I will never put any direct pressure on your uterus, and you can always ask any questions I hope you will be honest with me through every point of your treatment Massage is safe throughout every stage of your pregnancy and can help you with any aches and pains, stiffness and tension, and stress you may experience as your body and your baby grows and changes to make this the healthiest and happiest pregnancy and labour experience possible. I am currently accepting new patients on Wednesdays & Thursdays. I offer 30. 45, 60, and 90-minute treatments for massage therapy which include pre-natal, post-natal, and infant/pediatric patients. I would love to be a part of your journey and hope that I can help make it as smooth for you as possible. Click here to see my availability and to book an appointment References: Osborne, C., Kolakowski, M., & Lobenstine, D. (2021). Pre- and perinatal massage therapy: A comprehensive guide to prenatal, labor and post-partum practice. Handspring Publishing. “Infertility and Stress” – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6016043/ “Can Fertility Massage Help Get You Pregnant?” - https://www.whattoexpect.com/getting-pregnant/prepping-for-pregnancy/fertility-massage/ Authored by; Dr. Shannon Vander Doelen, ND
Naturopathic Doctor If you’ve been working with a fertility clinic to try to figure out why you haven’t had success in getting pregnant, receiving a diagnosis of Unexplained Infertility can be incredibly frustrating. On the one hand, you’re relieved to hear that “nothing is really wrong,” but on the other hand, you’re left with more questions than answers, and may not feel clear about the right next step. Though fertility clinics are often quite thorough in their initial assessment for a patient or a couple who have been trying to conceive, sometimes a few tests are overlooked, but may explain your infertility. Double check that you’ve had the following tests performed: Vitamin D Levels Vitamin D deficiency has been linked to many different health outcomes, including infertility. The sunshine vitamin serves so many roles in supporting us to get pregnant, starting with egg quality, our immune system function, our lining quality, and early embryo development, just to name a few. And just because you are taking a supplement or spend time outside does not mean your levels are adequate! A test is really the best and only way to determine your levels, and will allow you to supplement accordingly to boost your levels up into the optimal range. Thyroid Antibody Tests Autoimmune thyroid conditions have also been linked to infertility and miscarriage risk. Doctors will very often test our Thyroid Stimulating Hormone (TSH) levels, and if they are good, they may not look further. Our thyroid antibodies (called thyroid peroxidase antibody, or TPO, and anti-thyroglobulin, or anti-TG) can be elevated even in cases of normal TSH levels, and they can impact our fertility independently of TSH levels. It’s especially worth looking into these levels if you are experiencing secondary infertility (or trouble conceiving a second/subsequent child), as a previous pregnancy/postpartum experience can be taxing on your thyroid. CA-125 for Endometriosis Endometriosis is a condition where the tissue that is normally found inside the uterus is found outside of the uterus. It is thought that endometriosis can impact our fertility in numerous ways, from creating scar tissue, to overall creating a more inflammatory environment. Frustratingly, endometriosis cannot be seen on a standard ultrasound evaluation. And even more frustratingly, the severity of symptoms of endometriosis (pain mainly, with our periods, with urination/bowel movements, or with intercourse) don’t always correlate with the severity of disease, with some people not having any symptoms at all. CA-125 is a blood marker that when elevated, may indicate endometriosis. So when it is elevated, we can rule in endo (but if it is normal, we can’t necessarily rule out endo). Fasting Insulin Insulin is a hormone that manages our blood sugar when we eat. In general, we don’t want elevated levels of insulin relative to our blood glucose (this is referred to as insulin resistance). Testing our fasting insulin along with our fasting glucose, and then comparing the ratio between these values helps us assess for insulin resistance. Insulin resistance can negatively impact egg quality, ovulation, hormone levels, and implantation. Insulin resistance can be asymptomatic, but can also show up as non-specific symptoms like fatigue, stubborn weight loss, acne, cravings for sweet foods, and changes to skin pigmentation. Progesterone, Tested 7 Days After Ovulation I often see progesterone being tested along with our other Day 3 hormones. To be perfectly honest, the result of this test on this day is not particularly valuable, because our body only produces progesterone after ovulation, so we’re not usually expecting to have much progesterone in circulation on Cycle Day 3. However, we do want to make sure we’re getting a good progesterone surge approximately 7 days after ovulation to support the growth and maintenance of your endometrial lining, and to support implantation. So even if you’ve had your progesterone tested, double check which day of your cycle it was done on! If you have not had these tests done, you can definitely speak with your fertility clinic about them, or consider meeting and working with a Naturopathic Doctor who can facilitate a thorough initial assessment of your fertility and fertility history, and then recommend any testing that may be pending to help round out your fertility assessment to ensure you have ALL of the information you need to make an informed decision moving forward. I am currently accepting new patients and welcome you to book a free 30 minute meet and greet call so we can discuss your health and what options are available to you moving forward! Authored by; Dr. Arlene DubierNaturopathic Doctor & Birth Doula You may be wondering why your Naturopathic Doctor or Traditional Chinese Medicine Practitioner asks you about your cervical mucous every time you come in for an appointment, but trust me, it’s important! Your cervical mucous changes in texture, volume and colour at different parts of your menstrual cycle and these are changes can help you determine the time in which conception is most probable. This can also help for those of us who would like to be more in tune with our bodies and reproductive health. But I’m Already Using Ovulation Predictor Kits If you are using ovulation predictor kits (OPKs), these can track changes in luteinizing hormone (LH) levels. A surge in LH can indicate that ovulation is about to happen, but it does not indicate that ovulation has truly occurred. This is where either tracking basal body temperature (BBT) or cervical mucous changes can come in handy. BBT typically increases by 0.3-0.6 degrees Celsius on the day of ovulation. Tracking BBT is wonderful but can sometimes become challenging and potentially inaccurate, especially for those who have shift-work, travel frequently, or have trouble sleeping. What are the types of Cervical Mucous? Mucous or discharge is something which is produced by the cervix, and fluctuations in estrogen can trigger changes in this mucous to allow sperm easier access to the uterus for fertilization and implantation. From person to person, there can be slight variations in cervical mucous, but the most common could appear anywhere from:
Fertile Mucous The type of mucous which signifies that you are in your window of ovulation is the slippery mucous, which is similar in look and texture to raw egg-whites. As estrogen rises, this type of mucous can last from one to four days. How to Track Cervical Mucous This can be the part which people can be a little squeamish about, but as you practice you can get more comfortable checking cervical mucous. You can insert two clean fingers into your vagina and remove some mucous, checking the texture by squeezing your fingers together and then pulling them apart. Another, lower maintenance way of doing this is by simply wiping the vaginal area gently with toilet paper before urinating. If there is a slipperiness to the wipe, then you are likely experiencing cervical mucous. You can double check by looking at the toilet paper or any residual discharge on your underwear. The best thing you can do is either use a period tracking app which tracks cervical mucous, such as “Flo App”, or use a hand-written journal to track mucous changes. Using an app, will allow the algorithm to determine when you are most likely to have this fertile cervical mucous so you can time intercourse appropriately. However, it is important to keep in mind that most apps are slightly inaccurate by 1-2 days unless you have a textbook 28-day menstrual cycle. This is why, tracking ovulation via OPKs may also be used in tandem with cervical mucous tracking. How Accurate is Cervical Mucous? There can be some difficulties with cervical mucous accuracy, especially with regards to hydration or lack thereof which can give the appearance of lower volume of mucous. If there is an infection of the vaginal or urinary tract, there can also be foul smelling odour or a difference in colour. Additionally, the use of lubricants can also alter the ph of the vagina, if not ph-balanced or protected, and this can change the colour, texture and odour of the cervical mucous. Opt for fertility-friendly lubricants such as “Pre-Seed” by First Response to prevent changes in cervical mucous. Lastly, a past history of birth control usage can affect how “friendly” cervical mucous is to sperm. Being off the birth control pill for more than 3 months had a more positive effect on cervical mucous, than if women had been off the pill for a shorter period of time Cervical mucous is not the only form of fertility awareness that you should hang you hat on. There are a multitude of ways to track your fertile window, the most common being OPKs. However, as was previously mentioned, it is always best to couple an OPK with either basal body temperature and/or cervical mucous tracking. I offer a free consultation to all new patients. Book today to see me for a free 30 minute consultation. We can discuss any questions you might have on how best to track your fertile window, and how to improve your chances of conception. Wishing you all the best on your fertility journey! References:
1. Najmabadi, S., Schliep, K., Simonsen, S.E., Porucznik, C.A., Egger, M.J. & Stanford, J.B. (2021). Cervical mucus patterns and the fertile windown in women without known subfertility: a pooled analysis of three cohorts, Human Reproduction. 36(7), 1784-1795. 2. Oster, E. (2013). Expecting better: Why the conventional pregnancy wisdom is wrong and what you really need to know. Penguin Random House. The 4 Types of PCOS - authored by Dr Sarah DiMunno ND
If you are reading this article, you probably already know or suspect that you have PCOS, which stands for Polycystic Ovarian Syndrome. If you are thinking, “What the heck is that?” here is some background information. PCOS is a very common women’s health condition that leads to hormonal imbalances and a loss of ovulation. It is the number one reason women are diagnosed with infertility; and because of this it makes up a large portion of my practice. Diagnosis requires 2 of the following criteria:
Although not a diagnostic criteria the inability to lose weight deserves an honourable mention, and you’ll find out why a little later. As you can see the name of the condition is slightly misleading, you don’t necessarily need cystic ovaries to be diagnosed. Because of this misnomer many people focus too much on the presence or lack of cysts on the ovaries. Having cysts on their own isn’t enough to diagnose PCOS and you can still have PCOS if you don’t have cysts on your ovaries. If you were experiencing signs of high testosterone, also known as androgen excess, and a lack of ovulation, I’d be thinking about diagnosing PCOS regardless of cysts. If you do fit the criteria, the good news is this condition is 100% treatable. Figuring out the type of PCOS you have is the key to successful treatment. There are four types of PCOS, each with a slightly different root cause, making treatment approaches variable as well. Lucky for you, I’ve broke down each type below: Insulin-Resistant PCOS This is by far the most common and classic driver behind PCOS. Insulin is the hormone that is released in our body after eating; it brings blood sugar levels down. However, when you have insulin resistance your body doesn’t respond to the insulin released, and as a result your body starts producing more and more to keep your blood sugar levels normal. If you are susceptible to PCOS, these high levels of insulin will start preventing ovulation, make ovaries produce testosterone over estrogen, and boost luteinizing hormone (LH), which further reinforces the imbalance. If you have insulin-resistant PCOS, you have all the criteria of PCOS plus insulin resistance. You know you have insulin resistance if you struggle with maintaining a healthy weight and/or by measuring both your fasting blood sugar and fasting insulin in blood work. It’s important to address your insulin resistance because too much insulin can impair not only your cycle but can also contribute to heart disease, osteoporosis, and diabetes. Addressing insulin resistance is similar to treating diabetes and will respond very well to lifestyle changes like diet and exercise. Post-Pill PCOS This occurs after you stop taking birth control. To determine whether this is the type of PCOS you have, it is very important to take a look at what your period looked like prior to and following the birth control pill. If your period was irregular prior to starting the pill, you likely had PCOS the entire time, and didn’t know because the pill was masking your symptoms. If your period was normal, then your symptoms might be due to the pill and should return back to normal function after some time. It’s still important to investigate insulin resistance here because the pill can cause or worsen insulin resistance. If insulin resistance is present, then you have insulin resistant PCOS and should follow the instructions above. If insulin resistance is absent, then you can assume that with time and patience your hormones will return to normal. However, there are some things you can do to help ease the transition, including consuming adequate calories, and perhaps support a regular cycle using herbs or acupuncture. Inflammatory PCOS If you don’t have insulin resistance or the pill hasn’t negatively affected your periods, and you still have symptoms of PCOS then you might have inflammatory PCOS. This type of PCOS occurs when there is a lot of inflammation present in the body and past exposure to environmental toxins (who hasn’t been, am I right?!). Signs and symptoms of inflammation in the body include: IBS, unexplained fatigue, headaches, joint pain, and skin conditions like eczema and psoriasis. As you might have guessed the main goal for treating this type of PCOS is decreasing overall inflammation. Adrenal PCOS Lastly, if you don’t fit the criteria from any of the above categories then you might have adrenal PCOS. Chances are if you have this type of PCOS you are under A LOT of stress and you have been for some time (any professional students out there?). During the stress response, cortisol, our stress hormone, is released from the adrenal glands. DHEAS, another adrenal hormone, rises as cortisol does leading to high levels of DHEAS. When DHEAS is elevated, it can cause androgen excess as seen in PCOS. You should consider Adrenal PCOS if DHEAS is the only evidence of elevated androgen found and all other male sex hormones are normal. If you have this type of PCOS, you likely have a whole other whack of symptoms related to chronic stress like waking at night between 2-4 am, non-stop bloating, brittle nails and hair, low energy, etc. Since, this type of PCOS is largely driven by an abnormal stress response, treatment focus is on major stress reduction. If you feel like you don’t quite fit any of the descriptions above but have irregularities in your menstrual cycle, don’t fret. There are a number of other things to investigate including vitamin deficiencies & other hormonal imbalances that weren’t mentioned in this article. I offer a free consultation to all new patients. Book today to come in and see me for a free 30 minute consultation. We can discuss any questions you might have and I can give you some options for treatment. Getting off the pill - Authored by Sonam Patel RTCMP RAc - Registered Traditional Chinese Medicine Practitioner and Acupuncturist Are you someone who is planning on getting off the pill, but aren’t sure of what will happen to your body and menstrual cycles if you do? Maybe you want to work towards conceiving a child in the foreseeable future? Whatever your reason may be to discontinue your use of hormonal birth control, you might find yourself affected by the return of undesirable symptoms from before you began taking the pill, or new issues could arise. The intended purpose of oral contraceptive pills (OCPs) is of course to avoid pregnancy, but there are a number of other reasons that doctors prescribe them. Women who are experiencing severe cramps, heavy periods, or acne are given this type of medication in order to relieve their symptoms. One issue with this is that although it appears as though the problem has been fixed, it is only being temporarily managed. In other words, you’re putting a bandaid on it and the root cause is not being addressed. Secondly, taking these pills comes with the possibility of developing a number of side effects, including headaches/migraines, weight gain, decreased libido, or mood changes (not to mention the associated higher risk of serious health issues like blood clots and breast cancer). Furthermore, simply discontinuing the use of OCPs does not necessarily mean you are in the clear. Many women experience post-pill symptoms that they never dealt with even before taking them. Types of birth control pills There are many brands of OCPs out on the market, but do you know how they differ from one another? Doctors don’t always take the time to explain why they are prescribing a certain type of pill, and not a lot of women realize that there is a difference, or even how they are really going to be affected by them. Hormonal birth control pills are made up of synthetic forms of certain hormones to mimic the naturally-occurring ones that are produced by our own bodies. They include estrogen, progesterone (progestin is the synthetic form), or a combination of both. Most commonly, combination pills are given in 21 day packs, followed by 7 days of sugar pills to mark the days in the cycle (or no pills if you can remember when to start the next pack). The ratio of each component within the pills in one pack separate them into mono-, bi-, and even triphasic types. With monophasic pills, the ratio stays the same across the 21 days. Biphasic and triphasic types have 2 and 3 different ratios (respectively) of estrogen to progestin components. These pills must be taken with care, in the appropriate order to work as intended. The advantage with phasic pills is that an overall lower dosage of synthetic hormones is administered, which in turn can decrease the possible side effects or their severity. How do they work? As mentioned above, OCPs deliver synthetic hormones into your body. These imposters cause the hormone receptors in your body to detect estrogen and progesterone, effectively shutting down your natural production of them. This is not “regulating” your hormones or “fixing” your periods, but just duping your body into thinking it’s doing the job it was meant to do and not allowing it to properly function! The hormones in the pills work to inhibit pregnancy by suppressing follicular development and ovulation. So if an egg is not released, then no embryo can be formed and implanted in the uterus, and therefore no chance of pregnancy. Additionally, the hormones thicken the cervical mucus to make it harder for the sperm to travel up the cervix, and thin out the endometrial lining so that it becomes a less nutrient-rich environment for implantation. However, there is always the chance of human error when it comes to taking a pill at (roughly) the same time every day, so as a method of contraception alone, it is not 100% fool-proof. A study showed that 9 out of 100 females got pregnant while incorrectly taking combination pills, but only 14% of the group was using it for non-contraceptive related reasons. The Aftermath Unfortunately, after being on OCPs for extended periods of time, women stop taking them and experience a plethora of issues including unbalanced hormones, digestive upset, and fertility problems. Directly after getting off the pill, many women have irregular cycles and may even go for months without a period (amenorrhea), making it very difficult to conceive. This can be combined with other issues such as acne, impaired metabolism & weight changes, diminished sex drive, altered mental state (and often depression), and the list goes on. Not only this, but a lot of essential nutrients in our bodies have been depleted, leading to other deficiencies. What can be done? First off - don’t panic, all hope is not lost. If you’re looking to find some natural solutions to combat those pill-induced consequences, here are some good starting points:
Are you interested in learning more about getting off the pill with natural support? Book your free 30 minute consultation with me today! References
Gebel Berg E. The Chemistry of the Pill. ACS Cent Sci. 2015 Mar 25;1(1):5-7. doi: 10.1021/acscentsci.5b00066. Epub 2015 Mar 23. PubMed PMID: 27162937; PubMed Central PMCID: PMC4827491 Cooper DB, Adigun R, Mahdy H. Oral Contraceptive Pills. [Updated 2019 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. PMID: 28613632; ID: NBK430882 Bartlett E & Erlich L. Feed Your Fertility: Your Guide to Cultivating a Healthy Pregnancy with Chinese Medicine, Real Food, and Holistic Living. 2015 Fair Winds Press Your Natural Guide to an Easier Egg Retrieval Did you know that the egg retrieval procedure is considered minor surgery? Not to worry though, you’ll be sedated! (Which means don’t go alone, you’ll need someone to drive you home.) This blog is filled with tips and tricks to get you through the procedure with knowledge and ease. No surprises here! What’s happening exactly? Your eggs are typically retrieved through transvaginal ultrasound aspiration (the same ultrasound you’re already used to.) A fine needle is inserted into the ovaries to extract the eggs. In certain circumstances, the ovaries are accessed through the abdomen through laparoscopic surgery. The procedure itself typically takes 30 minutes. Sperm is retrieved at the same time, so make sure your partner abstains for the recommended amount of time and is ready to provide a sample! You will need to take the day off for the procedure as you’ll be recovering from anesthesia and experiencing a moderate amount of cramping. Many people find that they need a few days off work to be able to fully recover. Is there anything to do to prepare? Of course! Here are my top tips on how to prepare for the egg retrieval procedure, and recover like a champ Before the Egg Retrieval 1. Sleep peacefully You’ll have a faster recovery when your body is well rested, but you might be nervous the night before! Ease your nerves with a few soothing yoga poses like lying with your legs up the wall, or doing some deep breathing in child’s pose 10 minutes before bedtime. 2. Stay hydrated Dehydrated tissues are more sensitive and pain medications & anesthesia can cause dehydration. I know you’re used to those full bladder ultrasounds so you should be a water drinking pro by now! 3. Pack your diet with fiber Pain medications & anesthesia can also cause constipation. If you eat lots of fiber in the days leading up to the retrieval it will make going to the bathroom a lot easier. Incorporate foods like chia, flax, oatmeal, fruits and veggies, lentils, chickpeas, quinoa… the list goes on. While you’re eating those fiber rich foods, prepare your meals for the day of your retrieval ahead of time (or better yet get someone else to make them for you) to make healthy eating easier. 4. Stay calm with breathing techniques and meditation You’ll have to be at the clinic early. You can use the wait time to keep yourself calm and centered. There are so many amazing apps you can download that will guide you through quick and easy relaxation techniques to try before the procedure begins. Some of my favourites are: Headspace, Calm, and Aware. 5. Go for regular acupuncture If you’ve read my other blogs you’ll already know the incredible benefits of acupuncture for IVF. Not only will it improve the delivery of meds and nutrients to the pelvis with ample blood flow, it will ease your recovery after retrieval through tissue healing and relaxation. One to two sessions per week, leading up to the day of your retrieval, is ideal. If in extreme circumstances you cannot be sedated, acupuncture can be performed during the retrieval procedure for pain management. After the Egg Retrieval 1. Ready your heating pad & castor oil Expect to experience some mild to moderate cramping after the surgery. A heating pad can ease the muscle spasms. To make the relieving effects stronger, lather some castor oil over your pelvis and apply a cloth and heating pad over top. 2. Invest in ginger capsules You may be prescribed over-the-counter analgesic medications like Advil and Tylenol to ease cramping. Ginger is also an extremely effective analgesic/anti-inflammatory and in high doses does not cause bowel or gastrointestinal symptoms. It will also ease any post-surgery nausea. 3. Have some organic pantyliners handy You might notice a little bit of spotting the day of the surgery. I find organic liners to be a lot less irritating than conventional liners. Treat yourself to some new ones! 4. Cue up your favourite movies Some people won’t need to take more than one day off to recover, but you will need at least the day of surgery to recuperate. Get in your PJs and slippers and enjoy your favourite chick flicks and Netflix B-list movies (does anybody else watch those but me?) 5. Get some more acupuncture Here it is again! You’ve already done 12 sessions of acupuncture to optimize your eggs, now acupuncture can be used to relieve post-surgery symptoms. If you’re experiencing constipation, nausea, cramping, bloating, etc. acupuncture is your best friend. The more in-control and in-the-know you are regarding the egg retrieval process, the better you will feel. We’re here to support you every step of the way. We offer a free 30 minute consultation to all new patients. Call us today to book your appointment to find out more about how we can help you increase your chances of a smooth and successful egg retrieval. You can also book online! Written by Dr Caleigh Sumner ND
You know the drill when it comes to hormonal blood work; it’s a lot of poking and prodding on multiple days of your menstrual cycle. In my experience, my patients have had all the right testing done (mostly), but no one has taken the time to sit down with them and explain what the results truly mean. The biggest pitfall of serum (blood) hormone testing is that the reference ranges are MASSIVE. Which means it is highly unlikely that your results will be deemed “abnormal” even though you know something is wrong. So that’s what this blog is for; I’m going to break it all down for you and discuss what the results mean and the REAL range you’re looking for. Note: the following reference ranges are for women and are Canadian units. 1) Estradiol What it is: Estradiol, along with LH and FSH, stimulate follicle (egg) maturation. It’s also responsible for female sex characteristics, thickening of the endometrial lining, and bone protection. Estrogen can also be converted from fat, in both males and females, by an enzyme called aromatase. What it means: Low estradiol is present in peri-menopause and menopause. Elevated estrogen is present in early premature ovarian insufficiency (followed by low levels), and in estrogen dominant conditions like: PMS, endometriosis, PCOS, and obesity. Reference Range: Follicular 77-921 pmol/L Luteal 77-1145 pmol/L The “real” range: The width of the above ranges is ridiculous! Estradiol should be tested on day 3 and should be lower than 200 pmol/L and higher than 80 pmol/L. A level higher than this is a sign that the body is trying too hard to stimulate egg development, and the ovaries are not responding. In this case, you will likely see elevated FSH too. 2) FSH (follicle-stimulating hormone) What it is: The name says it all. FSH is in charge of the development and maturation of follicles. What it means: High levels are diagnostic of menopause, ranging from 27-133 IU/L. When your body is pumping out more FSH than normal, it’s a sign that the ovaries are not responding (just like estrogen). Low levels of FSH are typically present in PCOS. Reference Range: Follicular 3-8 IU/L Mid-cycle 3-22 IU/L Luteal 1.5-5.5 IU/L The “real” range: Higher than 8 IU/L on day 3 (that’s the 3rd day of your period) is too high and the value is only going up from there. 6 IU/L is as good as it gets on day three. 3) LH (Luteinizing hormone) What it is: Ah, the hormone everyone knows and loves! The LH surge triggers ovulation and is measured by urine strips. LH also contributes to the maturation of eggs. You may not know that estrogen surges right before LH, which can also be used to detect ovulation. What it means: On day 3, an LH to FSH ratio greater than 2:1 is indicative of PCOS. LH is elevated in PCOS for so many reasons I’ll need to dedicate another blog to it. Elevated LH also stimulates elevated testosterone production, and in turn estrogen production. Contrary to what you may think, high LH actually inhibits ovulation instead of stimulating it. Reference Range: Follicular 2-12 IU/L Mid-cycle 8-90 IU/L Luteal 1-14 IU/L The “real” range: LH should be almost equivalent to FSH on day 3. 6-8 IU/L is ideal. 4) Progesterone What it is: Most of the body’s progesterone is produced by the outer coating of the egg, called the corpus luteum. After you ovulate, progesterone levels increase to maintain the endometrial lining and prepare for embryo implantation. Progesterone also stimulates the production of a thick mucous that covers the cervix so no sperm can enter the uterus (FYI this is the basis of hormonal birth control). What it means: A low level of mid-luteal progesterone indicates anovulation and luteal phase defect (short luteal phase) and predicts implantation failure/ early miscarriage. Reference Range: Luteal 4-50 nmol/L The “real” range: On day 21 the minimum value is 10 nmol/L to have ovulated and 20 nmol/L to carry a pregnancy. Day 21 is arbitrary if you don’t ovulate on day 14. Progesterone is best-tested 7 days after you ovulate. 5) Prolactin What it is: The main function of prolactin is to stimulate breast milk production. However, elevation can also occur due to the following: benign pituitary tumor, periods of high stress, hypothyroidism, PCOS, and certain medications. What it means: Elevated prolactin inhibits the release of GnRH, which then inhibits the release of LH and FSH. Without LH and FSH, follicles will not develop. Reference Range: 5-30 ug/L The “real” range: Prolactin levels as high as 50 ug/L can inhibit ovulation, but small increases by a few points are relatively harmless. One-time elevation should be followed by repeat testing. As mentioned, stress is a major influence on this hormone. 6) DHEA What it is: A precursor hormone to both estrogen and testosterone. What it means: DHEA is often evaluated in PCOS, as elevations in this hormone increase androgen levels. It may be prescribed to improve ovarian reserve (but not without fun side-effects). Reference Range: <9.8 umol/L 7) Androstenodione What it is: Produced from DHEA, this hormone is the precursor to testosterone. What it means: Elevated androstenedione is found in PCOS and adrenal hyperplasia. Both conditions inhibit ovulation. It may be elevated in isolation, or with testosterone. Reference Range: Follicular 1.2-8.7 nmol/L Luteal 1.1-8.2 nmol/L 8) Testosterone What it is: You know this hormone for its role as the primary male sex hormone, but it’s important for women too! In the ovaries, testosterone is produced by the stromal cells and converted to estrogen. It participates in follicle growth and development, not to mention male and female libido. What it means: Too much is present in PCOS which is far from ideal, but too little can inhibit ovulation and egg development. Reference Range: Total testosterone 0.3- 1.8 nmol/L (some labs up to 4 nmol/L) The “real” range: Testosterone is extremely tricky to test accurately. Free testosterone is a better measurement than total and the reference ranges (depending on the lab) have huge variability. In order to test free testosterone you need to test total testosterone and sex hormone binding globulin. 9) AMH (Anti-Mullerian Hormone) What it is: It’s a hormone that can depict the female egg reserve because it is secreted by the eggs in the ovaries. The more eggs you have, the higher the value will be. Not surprisingly, AMH decreases with age. This is the only hormone test we have for predicting ovarian reserve. What it means: A lower value for your age means you have a lower number of eggs than the average female. A much higher value for your age is indicative of PCOS, as the cystic ovaries in PCOS secrete excess AMH. Reference Range: The numbers are averages based on age: < 33 = 2.1 ng/mL 33-37 = 1.7 ng/mL 38-40 = 1.1 ng/mL > 41 = 0.5 ng/mL The “real” range: At any age, a value > 3.15 - 4.45 ng/mL warrants further testing for PCOS. A value of 6.8-10 ng/mL is diagnostic. 10) TSH (thyroid stimulating hormone) & Antibodies (anti-TPO, anti-TG, anti-TSH) What it is: TSH is released by the anterior pituitary, which then stimulates the release of thyroid hormones (T3, T4) from the thyroid gland. TSH above the reference range with symptoms present is diagnostic of hypothyroidism, and below is hyperthyroidism. TPO and TG antibodies cause the thyroid condition known as Hashimoto’s, anti-TSH is more commonly present in Graves’. What it means: Deficient thyroid function affects egg quality, embryo quality, and implantation rates. Combine that with thyroid antibodies, and there’s an increased risk of miscarriage. Reference Range: TSH 0.32-4.0 mIU/L Antibodies should all be negative The “real” range: TSH should be < 2.5 to prevent miscarriage. A full thyroid lab panel (with individual thyroid hormones) is certainly necessary in cases of recurrent miscarriage. Have more questions? Meet with me! Wondering about your own lab results? Need a little help wading through the information and finding the useful parts? I offer a free 30 min consultation to all new patients. Click below to book yours today. I look forward to seeing you soon! Written by Dr Caleigh Sumner ND References
Zadehmodarres S, Heidar Z, Razzaghi Z, Ebrahimi L, Soltanzadeh K, Abed F. Anti-mullerian hormon level and polycystic ovarian syndrome diagnosis. Iranian Journal of Reproductive Medicine. 2015;13(4):227-230. Wiweko B, Maidarti M, Priangga MD, et al. Anti-mullerian hormone as a diagnostic and prognostic tool for PCOS patients. Journal of Assisted Reproduction and Genetics. 2014;31(10):1311-1316. doi:10.1007/s10815-014-0300-6. http://tests.lifelabs.com/Laboratory_Test_Information/Search.aspx Huhtinen K, Desai R, Ståhle M, et al. Endometrial and Endometriotic Concentrations of Estrone and Estradiol Are Determined by Local Metabolism Rather than Circulating Levels. The Journal of Clinical Endocrinology and Metabolism. 2012;97(11):4228-4235. doi:10.1210/jc.2012-1154. Kumar P, Sait SF. Luteinizing hormone and its dilemma in ovulation induction. Journal of Human Reproductive Sciences. 2011;4(1):2-7. doi:10.4103/0974-1208.82351. If you’re an adult female, you’ve probably been getting a regular screening PAP test completed every three years since your early 20’s. You book that often-dreaded appointment with your gynecologist or family doctor, and bring yourself in for a quick sample of cervical cells to be collected and sent off to the lab. Most of the time, this is the last you hear about your cervical health, until you’re reminded three years later to do it all again. For women who have abnormal cervical cells, however, this process tends to look a lot different. You are usually contacted by your gynecologists’ office, and informed that you will need to have a repeat PAP test much sooner than expected, usually in 3-6 months time. Depending on the extent of cellular abnormalities, you may also be referred for a colposcopy and biopsy of your cervix (fancy words for fancy imaging procedures). But how does all of this impact your fertility and future conception? Does the health of your cervix play a role in subfertility and pregnancy outcomes? With rates of HPV and cervical dysplasia on the rise, it’s important to be informed and empowered about how your cervical health can impact your fertility, even if conception is not your immediate goal. Today I break it all down, and chat about one of my favourite women’s health topics; cervical dysplasia! What does my abnormal PAP mean? Let’s start with the basics! My patient’s come in all the time, knowing nothing more than their PAP test result was “abnormal” – while this knowledge is important, it doesn’t tell us enough about how severe the cellular changes are, or how concerned we need to be about progression to cervical cancer. The presence of an abnormal PAP test generally indicates that you are experiencing some degree of cervical dysplasia – this means that under certain conditions and stressors, the previously normal cells of your cervix have mutated and become abnormal in size, shape, and/or function. The most common cause of these abnormal cellular changes is the Human Papilloma Virus (HPV), which has been estimated to be present in 80-90% of the North American Population at current. However, the interesting fact is that not all individuals who have been exposed to HPV will have abnormal PAP test results in their lifetime. A variety of factors seem to play a role in progression of HPV to cervical dysplasia, such as which specific HPV strain you have contracted (low or high risk), immune system function, sexual practices and HPV status of your sexual partners, as well as factors such as diet, smoking status, and long term oral contraceptive pill use. When your PAP test results return as “abnormal” they generally have one of the following basic terms to indicate the severity or “grade” of the cervical lesions present:
Huh? What is cervical dysplasia? Cervical dysplasia is a term used to describe the abnormal cellular changes that occur to the cells of the cervix. It indicates the presence of pre-malignant or pre-cancerous changes to the cervix, and if left untreated it may progress to cervical cancer over time. High stage lesions are more likely to progress to cervical cancer, while low stage lesions are less likely. The main causative factor is currently chronic HPV infection. What is HPV? HPV or the Human Papillomavirus is an infectious agent that is generally transmitted between sexual partners via direct sexual contact of the skin and/or mucous membranes. It is considered the main causative factor of cervical cancer worldwide. There are over 100 different strains of HPV, some of which can cause genital and non-genital warts, while others can cause cervical dysplasia and progress to cervical cancer. Low-risk strains of HPV (like 6 and 11) are more likely to cause external genital warts, while high-risk strains (like 16 and 18) are more often associated with cervical changes and progression to cancer. After your abnormal Pap test results, your gynecologist may assess for HPV strain using an HPV DNA test. How does this impact my fertility? Now for the fertility talk! Presence of cervical dysplasia on it’s own has not yet been linked to any changes to fertility status, but the use of recommended conventional treatment options is a different story. The most common conventional treatment of cervical dysplasia is a surgical procedure called LEEP, where the abnormal tissue is removed from the cervix using an electro-cautery tool. Research indicates that those who undergo surgical treatment of cervical intraepithelial neoplasia are at in increased risk of subfertility, with prolonged time to pregnancy. Time to conception was prolonged in 16.4% of women treated via surgical removal of the cervical tissue, versus 8.4% in untreated women, and 8.6% of women who underwent colposcopy alone. The LEEP procedure may also impact the production of cervical mucous, which is an extremely important aspect of how the sperm is able to travel unimpeded to meet and fertilise the egg during your fertile window. The procedure has also been linked to stenosis (or narrowing) of the opening to the cervix, which may impact fertility and pregnancy outcomes – most common of which include increased risk of premature rupture of membranes, low birth weight, and pre-term delivery. Incompetence of the cervix, which can be caused by surgical trauma to the area, may also increase the risk for miscarriage. The good news, is that LEEP is not your only option when it comes to treatment of cervical dysplasia. Luckily, the clearance rate of HPV and cervical dysplasia is naturally quite high – about 60% of individuals with low grade cervical dysplasia will regress to normal within two years, with 33% of those with high grade changes following suit. The main issue that arises is HPV persistence – conventional treatment options only focus on removing the abnormal cells from the cervix, and do not focus on clearing the virus itself. As a result, the return of cervical dysplasia post LEEP procedure can be as high as 30%. Naturopathic treatment options that improve clearance of HPV as well as promote regression of dysplasia fill in the gaps of conventional care, while also being mindful of impacts to future fertility and pregnancy outcomes. Top 5 Naturopathic Management Options for Cervical Dysplasia and HPV So, what can you do to help prevent persistence of HPV and improve clearance of dysplasia without impacting fertility? Ongoing PAP tests in accordance with screening guidelines are particularly important – whether you decide to move forward with conventional and/or naturopathic treatment, continued cervical screening is crucial in monitoring potential progression to cancer. Repeat PAP testing may also be linked to increased rate of regression of cervical dysplasia, so keep up to date on those PAP tests, especially if they’ve been abnormal!
We offer a free 30 minute consultation to all new patients. Come in and meet with one of our Naturopathic Doctors to discuss your options for promoting cervical health, while also preserving your fertility. Click the button below to book with us today! About the Author Dr Jennah Miller is a Naturopathic Doctor at the Toronto Reproductive Acupuncture Clinic. Read her full bio. References
De Vet, H. C. W., & Sturmans, F. (1994). Risk factors for cervical dysplasia: Implications for prevention.Public Health,108(4), 241-249. Tomita, L. Y., Roteli-Martins, C. M., Villa, L. L., Franco, E. L., & Cardoso, M. A. (2011). Associations of dietary dark-green and deep-yellow vegetables and fruits with cervical intraepithelial neoplasia: modification by smoking.British journal of nutrition,105(6), 928-937. González, C. A., Travier, N., Luján‐Barroso, L., Castellsagué, X., Bosch, F. X., Roura, E., ... & Sacerdote, C. (2011). Dietary factors and in situ and invasive cervical cancer risk in the European prospective investigation into cancer and nutrition study.International journal of cancer,129(2), 449-459. Kyrgiou, M., Athanasiou, A., Paraskevaidi, M., Mitra, A., Kalliala, I., Martin-Hirsch, P., ... & Paraskevaidis, E. (2016). Adverse obstetric outcomes after local treatment for cervical preinvasive and early invasive disease according to cone depth: systematic review and meta-analysis. Bmj, 354, i3633. Ciavattini, A., Clemente, N., Carpini, G. D., Gentili, C., Di Giuseppe, J., Barbadoro, P., ... & Liverani, C. A. (2015). Loop electrosurgical excision procedure and risk of miscarriage. Fertility and sterility, 103(4), 1043-1048. Acharya, G., Kjeldberg, I., Hansen, S. M., Sørheim, N., Jacobsen, B. K., & Maltau, J. M. (2005). Pregnancy outcome after loop electrosurgical excision procedure for the management of cervical intraepithelial neoplasia. Archives of gynecology and obstetrics, 272(2), 109-112. Bogdanova, J. (2008) Coriolus versicolor–innovation in prevention of oncogynecological diseases, especially HPV. Akush Ginekol (Sofiia). 2008;47 Suppl 3:51-3. Ali, N., Roshdy, E., Sabry, M., & Al-Hendy, A. (2013). Green tea: varieties, production and health benefits. Food and beverage consumption and health (Eds. Wu, W.), Nova Biochemical, USA, 33-74. Hudson, T., & Northrup, C. (2008). Women's Encyclopedia of Natural Medicine: Alternative Therapies and Integrative Medicine for Total Health and Wellness. McGraw-Hill. https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-fact-sheet#q2 There is so much that we don’t know about what it takes to carry a baby to term. If you’re working with a fertility clinic you’ll notice there’s a lot of observation during the first two weeks of your cycle, and once you’ve ovulated (or post embryo transfer) there’s not much monitoring after that! Rest assured, this article isn’t about what we don’t know but rather what we do! Fifty percent of miscarriages may not have an identifiable cause, but that means 50% of them do. Let’s go over the stats here for a moment. Recurrent miscarriage is considered two or more consecutive miscarriages, however diagnosis and treatment is often not suggested until three consecutive miscarriages have occurred. Not because you should have to suffer, or because your doctor doesn’t care, but because there’s a 15-25% chance of any pregnancy ending in miscarriage. The most common cause of miscarriage is fetal chromosome abnormality, which is about 60% of the time. While we’re going over the terminology, a “chemical pregnancy” is considered a miscarriage before 5 weeks, however I still consider it a miscarriage. Factors to consider in miscarriage:
Factors NOT to consider in miscarriage:
In my practice I don’t wait the “3-loss” rule to begin treatment and diagnosis, if you’ve experienced a loss and you want support, you deserve that support right away. Top 10 Most Common Causes of Miscarriage The majority of the list can be diagnosed with blood work or imaging. The entirety of the list can be treated!
Honorable mentions:
Have more questions? Meet with us! For any of the information we have provided, there are ways of diagnosing and treating these issues. You have options! We offer a free 30 minute consultation to all new patients Book yours today and lets get started! Written by Dr Caleigh Sumner ND References
Iqbal, S., Ghani, F., & Qureshi, R. (2016). Frequency of Thyroid Peroxidase Antibody and its Association with Miscarriages Among Pregnant Women. Journal of the College of Physicians and Surgeons Pakistan, 26(10), 831-834. Sundermann, A. C., Edwards, D. R. V., Bray, M. J., Jones, S. H., Latham, S. M., & Hartmann, K. E. (2017). Leiomyomas in pregnancy and spontaneous abortion: A systematic review and meta-analysis. Obstetrics & Gynecology, 130(5), 1065-1072. Bärebring, L., Bullarbo, M., Glantz, A., Hulthén, L., Ellis, J., Jagner, Å., ... & Augustin, H. (2018). Trajectory of vitamin D status during pregnancy in relation to neonatal birth size and fetal survival: a prospective cohort study. BMC pregnancy and childbirth, 18(1), 51. Loss, E. P. PRACTICE BULLETIN. EVALUATE, W. (2012). Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertility and Sterility, 98(5). El Hachem, H., Crepaux, V., May-Panloup, P., Descamps, P., Legendre, G., & Bouet, P.-E. (2017). Recurrent pregnancy loss: current perspectives. International Journal of Women’s Health, 9, 331–345. http://doi.org/10.2147/IJWH.S100817 No, G. T. G. (2011). The investigation and treatment of couples with recurrent first-trimester and second-trimester miscarriage. April 2011. Haas, D. M., & Ramsey, P. S. (2008). Progestogen for preventing miscarriage. Cochrane Database Syst Rev, 2. |
Copyright © Toronto Reproductive Acupuncture Clinic. All Rights Reserved | Privacy Policy












 RSS Feed
RSS Feed